Overview
A vasectomy is a simple, safe, and effective surgical procedure that makes a man unable to father a child (sterile), blocking the flow of sperm by obstructing the vas deferens in the scrotum. The testes will continue to produce sperm, but since the sperm have nowhere to go, they die and are absorbed by your body. Vasectomy is the most effective birth control method for men. The operation does not affect male hormone production or nerve supply to male organs. Therefore, neither the ability to perform sexual intercourse nor the sensations from it are affected in any way. Ejaculation of fluid occurs after the procedure, but without sperm. There are many good reasons for choosing to have a vasectomy, but it is a serious step. You and your partner should understand all the facts and share in the decision.
Is a Vasectomy Permanent?
Having a vasectomy should be considered a permanent decision. Before you make this choice, you must be sure it is what you want. Many men choose vasectomy because their families are already complete, but others have it as a means of reliable birth control. However, a vasectomy can be reversed with surgery in about 60-80% of cases provided it is done in the first ten years after the vasectomy. The success rate drops after that period of time. The cost of reversing a vasectomy is more expensive than the actual vasectomy, and is not a covered benefit by most insurance companies.
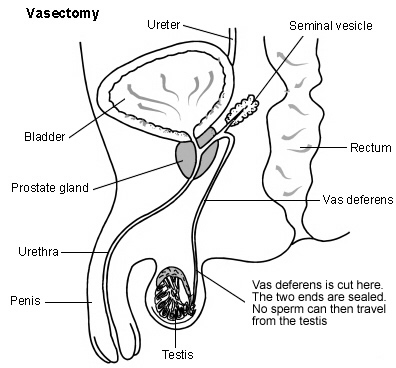
The Male Reproductive System
For pregnancy to occur, a man’s sperm (male reproductive cells) must join with a woman’s egg. To understand how a vasectomy works, you need to know how sperm are produced, stored, and released by the body.
- The urethra is the tube in the center of the penis. It transports both urine and semen. When you have an orgasm semen is ejaculated out of the urethra.
- The seminal vesicles and the prostate gland secrete fluids called semen. This white fluid helps nourish sperm and carry them along.
- The vas deferens are tubes that carry the sperm from the epididymis (a coiled tube that holds the sperm while they mature) to the penis.
- The testes are glands that produce sperm and male hormones.
Prior to the Procedure
Vasectomy is an outpatient (same day) procedure. In most cases, the procedure is performed in the physician’s office. To prepare for the procedure, please follow these steps:
- A consent form is necessary after you decide to have a vasectomy. The consent form states that you understand that there are certain risks involved and that the procedure cannot be guaranteed to make you sterile, although it is over 99% effective.
- Do not take aspirin, ibuprofen, or naproxen for 2 weeks before surgery. These medications can cause bleeding after the procedure.
- Arrange for an adult family member or friend to give you a ride home after the procedure.
- Your physician may ask you to shave your scrotum prior to the procedure.
- Eat no more than a light snack before surgery.
- Wear loose fitting clothes.
During Surgery
Please note: There are a variety of methods used to perform a vasectomy. Depending on your urologist, there may be a variation on your procedure. Each procedure is designed to effectively and efficiently cause sterilization.
The actual procedure takes between 15-30 minutes. First you will be placed on the exam table, and prepared with a soap solution. A local anesthetic is then injected into the skin of the scrotum. The local anesthetic acts immediately to numb the area. From this point on, moderate discomfort may occur during the procedure.
A small midline opening is made and the sperm tubes are individually mobilized, divided, and the remaining ends cauterized to complete the obstruction. The opening in the skin is closed with a stitch, which dissolves in 3 to 5 days. A gauze 4×4 patch and a scrotal supporter (jock strap) are supplied by our office.
After the Surgery
In the first 48 hours following surgery you should not lift heavy objects or strain. No sexual activity for 5-7 days. Add ice packs to the groin area for the first 12-24 hours after your procedure. Wearing a scrotal supporter day and night for approximately one week may help keep discomfort to a minimum. You may take a shower the following day.
Sex After a Vasectomy
After a vasectomy, some active sperm still remain in your semen. It will take time and many ejaculations before the sperm are completely gone. During this period, you must use another birth control method to prevent pregnancy. To make sure no sperm are left in your semen, you will need to have one or more semen examinations depending on your urologist’s protocol. You will likely be asked to collect a semen sample at home and bring it to our in-house lab, or an outside lab depending on your insurance. You are considered sterile when these samples show no evidence of sperm. Ask your urologist if additional follow-up is needed.
After You are Sterile
After your urologist tells you that you are sterile, you no longer need to use any form of birth control. However, a vasectomy does not protect you from sexually transmitted diseases (STDs).
Possible Risks and Complications
Vasectomy is a safe procedure, but there are risks, including bleeding and infection. You may also experience any of the following after surgery:
- Sperm granuloma is a small harmless lump that may form where the vas deferens is sealed off.
- Sperm buildup (congestion), which may cause soreness in the testes. Anti-inflammatory medications can provide relief.
- Epididymitis is inflammation of the epididymis that may cause scrotal aching. This often goes away without treatment. Anti-inflammatory medications and antibiotics can provide relief.
- In rare cases, the vas deferens can reconnect. This makes you fertile again and can result in an unwanted pregnancy.
- Sperm antibodies are a common response of the body to absorbed sperm. Antibodies can make you sterile, even if you try to reverse your vasectomy later.
- Long-term testicular discomfort may occur after surgery, but is very rare.
Post-Operative Instructions
Your vasectomy has been performed. There are one or two little incisions on each upper side of the scrotum. These were closed with sutures that are absorbable so you will not have to worry about having them removed. There will be soreness in the area for which you can take Tylenol or other medications that our doctor may give you. There is going to be a certain amount of swelling in the operative area. Deep inside, you might feel a little knot-like hard area of swelling. Occasionally, there may be a little ooze from the incision site. A dull aching pain may be experienced in the lower part of the abdomen or in the area of the groin. All of these are normal post-operatively, but should you be concerned, feel free to contact your doctor.
The following are suggested:
- Keep the operative area dry and covered for the first day. Apply an ice pack for the first day.
- Wear scrotal support for the first week.
- Starting tomorrow, you should take two (2) hot sitz baths a day for the first week.
- No intercourse for one week.
- Usually you can plan to return to normal activity after the first day, but avoid heavy lifting for one week if possible.
- You will need to use other methods of contraception until cleared by semen analyses at one and two months.
When to Call Our Office:
Call your doctor if you notice any of the following after surgery:
- Increasing pain or swelling in your scrotum
- Fever or chills
- Increasing redness or drainage of the incision
- Trouble urinating
Vasectomy Reversals (VasoVasotomy) Unfortunately, we don’t offer that specific procedure at our clinic.
Vasovasostomy (vasectomy reversal) is often the best option to restore fertility in men who have had a vasectomy. According to the National Institutes of Health (NIH), the number of men who undergo a vasectomy each year in the United States is approximately 500,000. This type of birth control is popular among adult males who are interested in preventing future pregnancies. For a variety of reasons, nearly 10% of men who undergo a vasectomy later decide to have it reversed. There are many factors that must be considered when deciding to have a vasectomy reversal.
The following are a few examples to consider:
- Vasectomy reversal is not a guaranteed procedure. The longer it’s been since your vasectomy, the less likely it is that your fertility will be restored.
- Even if sperm return to the semen, pregnancy is not guaranteed. Since your vasectomy, your body may have created sperm anti-bodies. These substances may prevent you from fathering a child, even if your sperm count returns to normal.
- Has your partner had fertility problems? If so, another procedure (such as in vitro fertilization) may be more likely to result in pregnancy.
Restoring the Flow of Sperm
Testicles make sperm, which are male reproductive cells. Sperm travel from the testicles to the penis through one of two tubes called the vas deferens. On the way, sperm mix with other fluids to form semen, which leaves the body during ejaculation. During a vasectomy, each vas deferens is cut, blocking sperm from leaving the body. This makes you sterile (unable to make a woman pregnant). A vasectomy can sometimes be reversed, restoring the flow of sperm out of the body.
How the Procedure Works
During a vasectomy reversal, the two cut ends of the vas deferens are stitched back together. With the sperm pathways restored, sperm can once again travel through the vas deferens and leave the body during ejaculation. You may then be able to father a child.
You will receive medication to keep you comfortable. This procedure is always done under anesthesia in our ambulatory surgery center located directly next door from our medical group. Once the anesthesia takes effect:
- An incision is made in your scrotum
- The cut ends of each vas deferens are lifted out and examined. A section of each cut end may be removed
- The end closer to the testicles is cut until fluid flows freely. This fluid may be looked at under a microscope to see if sperm are present.
- The two cut ends are stitched together. If needed, the vas may be attached directly to the epididymis (tissue behind the testicle)
- When both of the vas deferens are reconnected, the incisions in the scrotum are sutured closed.
Post-Operative Instructions
Activity
Physical activity is to be restricted immediately following your vasectomy reversal. This is particularly true during the first five days after surgery. During that time you should remain relatively inactive and avoid lifting objects heavier than 10 pounds. Apply an ice pack wrapped with a terry cloth towel directly to the scrotum off and on the first 48 hours. It is extremely important that you do not engage in sexual intercourse and do not ejaculate for at least three weeks following the surgery. The vas deferens must be kept “at rest.”
Diet
You may return to your normal diet immediately. It is suggested that you eat fresh fruits and vegetables (roughage) to avoid constipation.
Wound Care
As mentioned above, an ice pack should be applied to the scrotum off and on for the first 48 hours following surgery. You will go home with an athletic supporter and gauze fluffs to protect the scrotum and incision sites. The gauze should be changed on a daily basis for at least three or four days. You should wear an athletic supporter for 7-10 days since it will give you additional support and protection. You may shower at any time following the surgery, but avoid scrubbing the scrotum vigorously, and do not take tub baths until told to do so.
Medications
You may be discharged with a narcotic analgesic. If the pain is not too uncomfortable, then it is advisable to simply take Tylenol (acetaminophen) or Advil (ibuprofen). You may also be discharged with a five day supply of antibiotics, which you should take according to the directions on the bottle.
Please report the following problems to your urologist:
If you experience any of the following call our office as soon as possible.
- Fever over 101 degrees Fahrenheit
- Excessive swelling of the scrotum and/or bleeding
- Drug reactions (hives, skin rash, nausea, or vomiting)
Follow-Up
You will be given a post-operative follow-up appointment to see Dr. Leung within a couple weeks of your surgery. Since it takes over 70 days for sperm to develop, the first postoperative sperm analysis is not performed until 8-10 weeks following surgery. Please remember that it is very important that you do not ejaculate during the first three weeks following surgery.
Yuk-Yuen Leung , M.D
Aside from being a quality general urologist, Dr Leung joined Urology Associates several years ago to bring his micro surgery skills to Central California. Dr. Leung has a 99% success rate.
Dr. Leung is board certified by the American Board of Urology. At this time, he is our only urologist that performs the vasovasostomy procedure.
A graduate from the University of Texas at Austin in electrical engineering and then completing his Master’s Degree in Biomedical Engineering Dr Leung went on to Johns Hopkins University and The State University of New York for his medical education. While Johns Hopkins University, he was involved in progressive medical research using advanced engineering technologies. He built machines and computer systems to study biological processes, and in an effort to combine and apply his engineering and biomedical research background, he attended the State University of New York and graduated with a doctoral degree in Medicine with “Distinction in Research”.
Unfortunately, we don’t offer that specific procedure at our clinic